Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Contents
Swollen legs can be a distressing condition that can impede your daily activities. If left untreated, the condition can worsen over time. There are various diseases and underlying conditions that can lead to swelling in the legs below the knee. It is essential to identify the potential causes of this condition to seek appropriate treatment and management.
Leg swelling typically occurs due to fluid retention and inflammation. The accumulation of fluid in the legs, known as peripheral edema, is a common cause of leg swelling below the knee. Some of the common underlying conditions associated with leg swelling include:
Deep Venous Thrombosis (DVT) is a condition characterized by the formation of blood clots in the deep veins of the legs, most commonly in the deep calf vein. Symptoms of DVT include swelling, pain, and redness in the affected leg. Factors such as obesity and a sedentary lifestyle can contribute to the development of blood clots in the lower legs. Treatment for DVT often involves anticoagulant therapy.
May-Thurner Syndrome (MTS) is a condition that affects blood flow from the legs and pelvis to the heart. It is caused by the compression of the iliac vein, leading to tenderness and swelling in the legs. Symptoms of MTS may worsen with activity, and proper investigations are necessary for diagnosis and management.
Congestive heart failure can result in peripheral edema and leg swelling. In advanced stages of heart failure, patients may experience pulmonary congestion and fluid accumulation in the extremities. Lower extremity edema is a common symptom in heart failure patients, and different types of edema may be present, including pitting edema and peripheral edema.
Pulmonary hypertension, a condition characterized by high blood pressure in the arteries of the lungs, can also lead to leg swelling below the knees. Obese patients are more prone to developing bilateral leg edema in association with pulmonary hypertension. The link between pulmonary hypertension and heart failure can exacerbate edema in affected individuals.
Kidney diseases that impair the removal of sodium and water from the body can result in fluid accumulation in the legs, leading to peripheral edema. Critically ill patients are at a higher risk of developing acute kidney injury and subsequent leg swelling.
Lymphedema, characterized by the leakage of lymphatic fluid into the arms and legs, can cause tissue swelling. Abnormalities in the lymphatic system, cancer, and its treatment can trigger lymphedema, with leg swelling worsening upon standing.
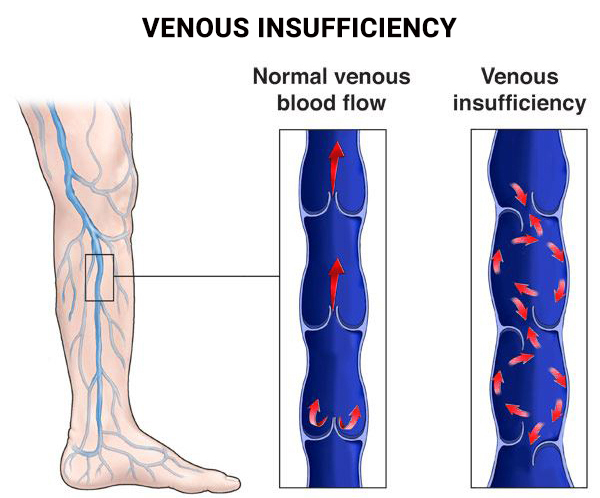
Varicose veins and chronic venous insufficiency are common venous conditions that can cause lower extremity edema. The pooling of blood in the legs due to impaired venous return to the heart can lead to leg swelling. Individuals with occupations that involve prolonged standing are at a higher risk of developing varicose veins.
During pregnancy, hormonal changes and increased pressure on the leg veins can result in swelling in the lower extremities. Approximately 50% of pregnant women experience swelling in the legs, ankles, and feet, accompanied by discomfort. It is essential to consult healthcare providers for appropriate management strategies.
Inflammatory conditions, injuries, and trauma can also contribute to leg swelling below the knee. Conditions such as arthritis, gout, bursitis, and cellulitis can lead to localized swelling and discomfort in the legs. Prompt medical attention is necessary to address the underlying causes of inflammation and swelling.
Managing leg swelling at home involves various self-care strategies to alleviate discomfort and promote recovery. Some effective tips for reducing leg swelling include:
Massaging the affected area with gentle pressure can help stimulate circulation and reduce fluid buildup. Applying a cold compress to the swollen area for 20 minutes several times a day can also help alleviate swelling and discomfort.
Wearing compression stockings can provide consistent pressure on the affected area, preventing fluid accumulation in the tissues. Keeping the affected leg elevated above heart level can facilitate the movement of excess fluid back towards the heart.
Over-the-counter anti-inflammatory medications can help reduce inflammation and alleviate pain associated with swollen legs. It is essential to follow the recommended dosage and consult a healthcare provider if necessary.
While mild leg swelling may resolve on its own, persistent or severe swelling requires medical evaluation. It is crucial to seek immediate medical attention if you experience symptoms such as difficulty breathing, chest pain, fever, or dizziness in conjunction with leg swelling. Healthcare providers may perform diagnostic tests such as X-rays or ultrasounds to identify the underlying causes of leg swelling and recommend appropriate treatment options.
Swollen legs from the knee down can be a result of various underlying conditions, ranging from venous disorders to inflammatory conditions and injuries. Understanding the potential causes of leg swelling is essential for timely intervention and management. By implementing preventive measures and seeking medical advice when necessary, individuals can effectively address leg swelling and improve their overall quality of life.