Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Contents [hide]
When it comes to blood transfusions, understanding blood types is crucial for ensuring compatibility and preventing adverse reactions. Blood types are classified into four main groups: A, B, AB, and O, with each group further categorized as positive or negative based on the presence of the Rh factor. This classification system helps healthcare providers determine which blood types can be safely transfused into patients in need.
The ABO blood group system is based on the presence of antigens on the surface of red blood cells. These antigens determine whether a person has blood type A, B, AB, or O. Depending on the combination of antigens present, individuals can have no antigens, A antigens, B antigens, or both A and B antigens. In addition to antigens, antibodies in the plasma play a crucial role in blood transfusions by identifying and destroying foreign antigens.
For example, individuals with type A blood have A antigens on their red blood cells and anti-B antibodies in their plasma. If they receive blood from a donor with type B blood, their immune system will recognize the foreign B antigens as threats and initiate an immune response, leading to potentially life-threatening complications.
In addition to the ABO system, the Rh blood group system classifies blood types as positive or negative based on the presence of the RhD antigen. Individuals who have the RhD antigen are Rh positive, while those who lack the antigen are Rh negative. This distinction is important for determining blood compatibility, especially in cases where Rh incompatibility can lead to severe reactions.
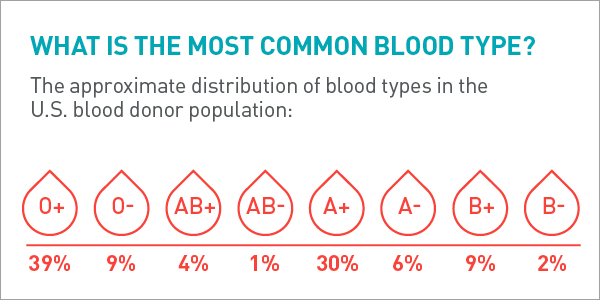
Among the various blood types, O negative blood is considered the universal donor due to its compatibility with all blood types. This makes it invaluable in emergency situations where the recipient’s blood type is unknown. Only 7% of the population has O negative blood, making it a high-demand blood type for transfusions, particularly in critical care settings.
On the other hand, O positive blood, while not universal, is the most common blood type, with 38% of the population having this blood type. O positive blood is often used in trauma cases and surgeries where the patient’s blood type is not immediately known. Its widespread availability and compatibility with other positive blood types make it essential for meeting the demand for blood transfusions.
Understanding blood type compatibility is essential for safe blood transfusions and organ transplants. Each blood type has specific compatibility requirements, with some types being universal donors or recipients. For example, individuals with type O negative blood can donate to individuals with any blood type, making them universal donors in times of urgent need.
Moreover, blood type inheritance follows genetic patterns, with individuals inheriting their blood type from their parents. This inheritance process results in a diverse range of blood types across populations, each with its unique characteristics and compatibility profiles.
As of 2024, the need for blood donations remains constant, with millions of blood components transfused each year in the United States alone. Blood donors play a critical role in replenishing the blood supply and meeting the demand for various blood types, especially those in high demand like O negative and O positive.
By donating blood, individuals can contribute to saving lives in emergency situations, surgeries, and treatments for various medical conditions. Blood donation centers rely on the generosity of donors to ensure an an adequate supply of blood for patients in need, underscoring the importance of regular donations to support healthcare systems.
Healthcare providers and blood banks prioritize blood type compatibility to prevent adverse reactions and ensure the safety of transfusions. By adhering to established protocols for blood typing and cross-matching, medical professionals can minimize the risk of complications and provide optimal care to patients requiring blood transfusions.
With advancements in blood typing technology and increased awareness of the importance of blood donation, healthcare systems can continue to meet the demand for diverse blood types and improve patient outcomes through safe and effective transfusion practices.